Book an Appointment
Learn how Regen Doctor is assisting patients in living life to the fullest.
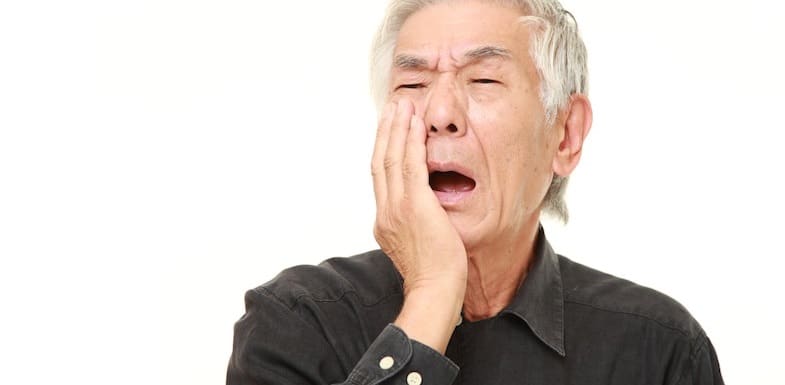
When a chronic pain syndrome is bad enough to earn the nickname “the suicide disease” because of an increase in suicide ideation among those who suffer from it, it’s important to learn all you can when you or a loved one receives a diagnosis. Also historically referred to as tic douloureux, Fothergill’s disease, prosoplasia, or trifacial neuralgia, trigeminal neuralgia (TN) is one of the most common and well-defined causes of severe facial pain. As common as it is, trigeminal neuralgia still remains one of the most challenging types of pain to treat. Here’s what you should know.
Trigeminal neuralgia is a complex pain syndrome that has its root cause in one particular nerve in your face. This nerve is located just in front of your ears on either side of the head. The trigeminal nerve, also known as the fifth cranial nerve, has three major branches.
All three branches supply parts of the meninges and bring sensory innervation to the face and motor innervation to the muscles that you use for chewing and swallowing.

There are a variety of trigeminal neuralgia causes. Pressure on the trigeminal nerve root is the leading cause of trigeminal neuralgia the majority of the time. This pressure may be due to a swollen, inflamed intercranial artery that is applying pressure to the area, or it may be due to some other injury or trauma. Sometimes the place where the nerve root enters the skull also becomes narrower, causing pressure.
Other causes of compression include the following:
As the compression of the trigeminal nerve continues, it can cause damage to the protective covering of the nerve called the myelin sheath. Once this myelin sheath is damaged, the nerve begins to respond unpredictably. As a result, the nerve can act in an erratic manner, causing pain at the trigger of a light touch, chewing, or brushing the teeth.
The symptoms of trigeminal neuralgia are unmistakable. Sudden, severe, stabbing, recurrent episodes of pain on one side of the face are the most frequent symptom. This pain occurs most often on just one side of the face but can occur on both.
Some patients also report a constant aching or burning sensation, or a tingling sensation or aching that precedes the pain episodes.
Pain can be triggered by the slightest contact, including the following:
Any vibration or contact with the face, eyes, head, or mouth may trigger the intense flashes of pain. The attacks usually last several seconds to a couple of minutes and repeat over subsequent hours to weeks. The episodes then disappear for months to years before recurring.
Pain rarely occurs at night during rest, and trigeminal neuralgia tends to affect women slightly more than men at a ratio of 1.5:1. The chances of developing trigeminal neuralgia increase slightly with age, with attacks worsening over time and remission periods becoming more infrequent and shorter in duration.
Trigeminal neuralgia is diagnosed in an estimated 40,000 people in the U.S every year. This may seem like a small number, but given that the rate of suicide and suicidal ideation is higher than the national average due to the severe pain episodes, proper diagnosis and treatment is crucial.
Diagnosis of trigeminal neuralgia is made clinically based on a thorough patient history and medical examination. Keeping a record of your pain episodes, including type, quality, length of time, and triggers, can help you get a more accurate diagnosis.
Other diagnostic criteria for classic trigeminal neuralgia have been developed and published by the International Headache Society (IHS). They include:
Much of the diagnosis is a process of eliminating the possibility of other conditions causing pain. Your doctor may order radiological imaging depending on their clinical suspicion and your medical history.
Other causes of facial pain can be postherpetic pain, which usually occurs with a persistent rash that involves the ophthalmic branch. It may also be a form of migraine pain, which is usually more prolonged and often throbbing. If a tumor is present, or high blood pressure or stroke is suspected, your treatment options will be much different. This is why eliminating other issues is crucial.
It can be difficult to diagnose trigeminal neuralgia. Many sufferers are misdiagnosed with migraine pain and may wait years for proper diagnosis and relief. It is important to find a pain specialist who has received specialized training to examine and diagnose trigeminal neuralgia.
Trigeminal neuralgia is just as challenging to treat as it is to diagnose. When you do receive a diagnosis, it’s important to start treatment right away. If an underlying condition is causing your pain (e.g., multiple sclerosis), treatment of that usually occurs simultaneously with treatment for trigeminal neuralgia.
There are four types of trigeminal neuralgia treatments.
Anti-inflammatory, anticonvulsant, and antidepressant medications are often the first approaches for treating trigeminal neuralgia pain, as they are non-invasive and have manageable side effects.
Carbamazepine is the most effective of these options for most patients. If carbamazepine is ineffective or not tolerated, then gabapentin, phenytoin, baclofen, lamotrigine, topiramate, or tizanidine may provide relief.
Most pain physicians recommend periodically tapering medications down in patients experiencing pain relief in order to check for the occasional permanent remission.
Local anesthetic blocks may occur after or in conjunction with prescription medication, but they only provide temporary pain relief.
Glycerol injections are not an anesthetic injection but can provide pain relief by intentionally damaging the nerve to block painful signals. When this is effective, you can typically repeat the injections every year or two.
When more conservative treatment options fail, surgery may provide relief. There are a variety of surgical procedures that can help, including:
All of the above mentioned treatments have a high recurrence of pain.
Peripheral nerve stimulation (PNS) or spinal cord stimulation (SCS) are minimally-invasive treatment options that replace pain signals with a mild tingling sensation. These treatments may offer the potential for long-term management of pain without invasive treatment or prescription medications. Because there is a trial period for SCS or PNS, these procedures are less invasive, reversible, adjustable, and testable for patients in pain.
Some patients also experience short-term pain relief with acupuncture, while others learn to manage their response to pain using biofeedback or meditation. While biofeedback and meditation do not “cure” the underlying cause of your pain, they can help you to feel more equipped to manage it when it flares up.
If If you have any questions or are simply looking for more information please contact us and our friendly team will be happy to answer your questions and help in any way we can.
