Spinal stenosis is a painful condition that affects an estimated half a million people in the U.S. From a mild annoyance to a debilitating disorder, spinal stenosis can impact your everyday life with pain and limited mobility. Here’s what you should know about this condition.
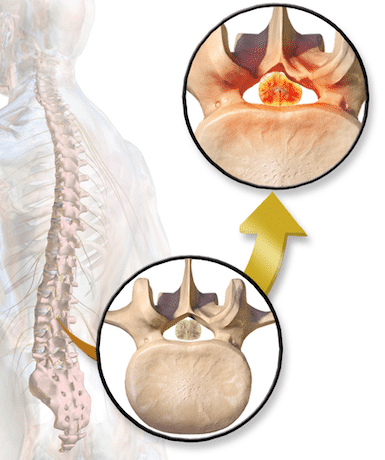
Spinal stenosis is the name for the narrowing of the spinal canal. It is most common in the lumbar region of your back but can also occur in the neck. The narrowing of the spinal canal leads to compression, which can cause painful nerve and spinal cord impingement.
The most common symptom of spinal stenosis is persistent pain in the lower back and lower extremities (i.e., sciatic pain). Difficulty walking, numbness and tingling in the legs and feet, and a decrease in physical activity may also occur.
Spinal stenosis most commonly affects people over the age of 65, and scoliosis and hypertension are often risk factors.
The spinal column is paradoxically a strong support system for the body and a vulnerable weak link. An estimated 80% of people in the U.S. will experience significant back pain in their life, some of it due to the anatomy of the spine.
The individual vertebrae (bones of the spine) provide a flexible support structure while also protecting your spinal cord. Separating each individual vertebrae are intervertebral discs that act as cushions to minimize the impact the spinal column receives. Since the discs are soft and provide support, they have a tendency to herniate backwards through the outer disc segment and ligaments. This can cause irritation to the spinal cord and adjacent nerves.
There are also ligaments that attach to each vertebrae and provide strength and mobility to the spine as well as the many groups of muscles that are responsible for movement of your spine. Nerves attach to the spinal cord and exit the spine to innervate the skin, muscles, and surrounding structures of the back and lower extremities.
In spinal stenosis, symptoms occur when the narrowing of the spinal canal begins to affect the nerves and the spinal cord itself. If there are any underlying issues in the spine (e.g., herniated discs) that are already causing problems, the condition is made worse by a narrower spinal column. Disc bulging and disc herniation as well as arthritic changes can cause narrowing.
The most common cause of spinal stenosis is unavoidable: age.
As we age, gravity begins to do its work on us. Our posture becomes a bit stooped, and we may begin to lose bone or have less dense bone. Getting older does not guarantee you will develop spinal stenosis, but it is one of the main causes of it.
In addition to the pain and symptoms above, another common complication of spinal stenosis is central sensitization. When spinal stenosis becomes chronic, the peripheral nervous system (PNS) and the central nervous system (CNS) lose the ability to accurately gauge stimuli. The PNS is more active due to inflammation in the nerves, so when stimulated, it sends unnecessary messages to the CNS. Eventually normal inputs from the PNS begin to produce abnormal responses. A light touch might produce significant pain.
A serious complication of severe progressive spinal stenosis is nerve stimulation involving bladder or bowel incontinence, lower extremity weakness, or loss of sensation. If you experience these symptoms, consider them a medical emergency and head to your doctor or emergency room.
To diagnose spinal stenosis, your doctor will take a thorough medical history and complete a physical exam. Your doctor looks for tenderness or sensitivity over certain areas of the spine and gauges your pain-free range of motion in your legs.
A CT scan or MRI can help your doctor see the narrowing of the spine, even if an X-ray is not able to pick it up. Currently MRIs are the standard of care to visualize and diagnose chronic back pain and are used before any treatments begin.
Spinal stenosis treatments are as individualized as the people with the condition. Here are seven treatments to consider with your doctor.
1. Exercise
Exercise can work both as treatment and prevention of spinal stenosis.
In the acute phase of this condition, rest may be recommended, but spinal stenosis exercises can provide profound pain relief.
2. Medications
NSAIDs (ibuprofen and naproxen sodium), membrane stabilizing drugs, and other analgesics are often used in the management of pain associated with spinal stenosis.
These may only be useful in the acute phase, as other non-pharmacological interventions have been shown to be more effective. Opioids are not recommended for spinal stenosis pain.
3. Epidural steroid injections
This procedure involves injecting a medication into the epidural space where irritated nerve roots are located. This injection includes both a long-lasting steroid and a local anesthetic (e.g., lidocaine or bupivacaine). The steroid reduces inflammation and irritation while the anesthetic interrupts pain transmission long enough to let the steroid get to work.
The combination medicine then spreads to other levels and portions of the spine, reducing inflammation and irritation. The entire procedure usually takes less than 15 minutes. Epidural steroid injections (ESI) are effective at rapidly relieving symptoms so that you can become active again. This allows you to undergo other therapies, like physical therapy, to address the underlying cause of your pain.
4. Percutaneous adhesiolysis
Adhesiolysis, also known as the Racz procedure, removes excessive scar tissue in the epidural space. Scar tissue originates from inflammation, irritation, and often surgery and can increase the pain of spinal stenosis.
For this procedure, a needle is inserted into the caudal epidural space (by the tailbone) and a catheter is advanced into the epidural space under fluoroscopy guidance. Corticosteroid, local anesthetic, wydase, and hypertonic saline are injected to aid in lysing (or breaking) the adhesions (scar tissue).
5. Spinal cord stimulation
Our team also offers spinal cord stimulation for the treatment of spinal stenosis. A study of people with severe spinal stenosis who received spinal cord stimulation found a 69% improvement rate in lowered pain scores, a decrease in medication use, and improved quality of life.
An electrical device implanted in the lumbar spine decreases your perception of pain by confusing the spinal cord and brain pain processing centers. Initially, your doctor will use a trial stimulator to see if this device will help you long-term. They’ll place a small electrical lead in the epidural space and, if the device works, a mild tingling will replace your pain sensations.
If you have success in your trial, you may decide to have a permanent SCS device implanted.
6. Complementary alternative medicine
Complementary treatments can help relieve pain and relieve stress, typically alongside traditional treatments. In 2012, a large meta-analysis of studies involving 18,000 patients found that acupuncture decreased pain in a statistically significant way for the majority of patients.
Other holistic spinal stenosis treatments include controlling stress through breathing and meditation. While these treatments don’t fix the structural issue in your back, they can help you deal with any symptoms you experience while undergoing other treatments.
7. Surgery
Most doctors agree that it’s important to start with conservative treatments for spinal stenosis. When all conservative measures have been exhausted and the symptoms persist, a more invasive surgical procedure (e.g., a laminectomy or foraminotomy) may be necessary to take pressure off the spinal cord and surrounding nerves.
For patients who rapidly develop loss of bladder/bowel function, weakness, and decreased sensation, this type of emergency surgery may need to be performed to prevent further complications.
If you have any questions or are simply looking for more information please contact us and our friendly team will be happy to answer your questions and help in any way we can.
